Sensory processing disorders (SPD) are more prevalent in
children than autism and as common as attention deficit hyperactivity
disorder, yet the condition receives far less attention partly because
it’s never been recognized as a distinct disease.

Pratik Mukherjee, MD, PhD
In a groundbreaking new study from UC San Francisco, researchers have
found that children affected with SPD have quantifiable differences in
brain structure, for the first time showing a biological basis for the
disease that sets it apart from other neurodevelopmental disorders.
One of the reasons SPD has been overlooked until now is that it often
occurs in children who also have ADHD or autism, and the disorders have
not been listed in the Diagnostic and Statistical Manual used by
psychiatrists and psychologists.
“Until now, SPD hasn’t had a known biological underpinning,” said senior author
Pratik Mukherjee,
MD, PhD, a professor of radiology and biomedical imaging and
bioengineering at UCSF. “Our findings point the way to establishing a
biological basis for the disease that can be easily measured and used as
a diagnostic tool,” Mukherjee said.
The work is published in the open access online journal
NeuroImage:Clinical.
‘Out of Sync’ Kids
Sensory processing disorders affect 5 to 16 percent of school-aged children.
Children with SPD struggle with how to process stimulation, which can
cause a wide range of symptoms including hypersensitivity to sound,
sight and touch, poor fine motor skills and easy distractibility. Some
SPD children cannot tolerate the sound of a vacuum, while others can’t
hold a pencil or struggle with social interaction. Furthermore, a sound
that one day is an irritant can the next day be sought out. The disease
can be baffling for parents and has been a source of much controversy
for clinicians, according to the researchers.

Elysa Marco, MD
“Most people don’t know how to support these kids because they don’t fall into a traditional clinical group,” said
Elysa Marco,
MD, who led the study along with postdoctoral fellow Julia Owen, PhD.
Marco is a cognitive and behavioral child neurologist at UCSF Benioff
Children’s Hospital, ranked among the nation's best and one of
California's top-ranked centers for neurology and other specialties,
according to the 2013-2014
U.S. News & World Report Best Children's Hospitals survey.
“Sometimes they are called the ‘out of sync’ kids. Their language is
good, but they seem to have trouble with just about everything else,
especially emotional regulation and distraction. In the real world,
they’re just less able to process information efficiently, and they get
left out and bullied,” said Marco, who treats affected children in her
cognitive and behavioral neurology clinic.
“If we can better understand these kids who are falling through the
cracks, we will not only help a whole lot of families, but we will
better understand sensory processing in general. This work is laying the
foundation for expanding our research and clinical evaluation of
children with a wide range of neurodevelopmental challenges – stretching
beyond autism and ADHD,” she said.
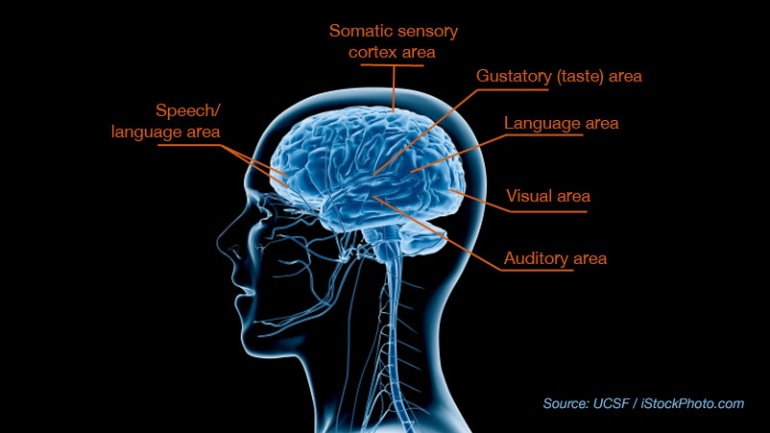
Imaging the Brain’s White Matter
In the study, researchers used an advanced form of MRI called
diffusion tensor imaging (DTI), which measures the microscopic movement
of water molecules within the brain in order to give information about
the brain’s white matter tracts. DTI shows the direction of the white
matter fibers and the integrity of the white matter. The brain’s white
matter is essential for perceiving, thinking and learning.
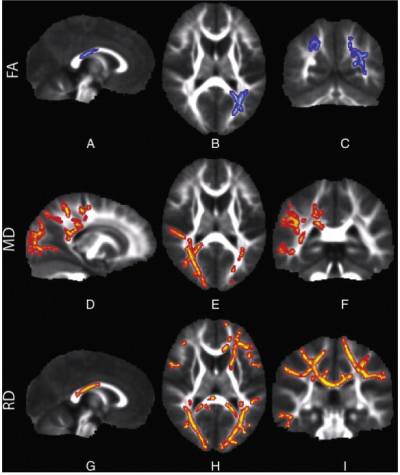
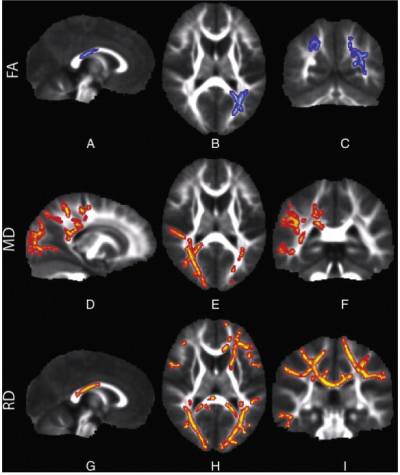
These brain images, taken with DTI, show water diffusion within the
white matter of children with sensory processing disorders.
Row FA:
The blue areas show white matter where water diffusion was less
directional than in typical children, indicating impaired white matter
microstructure.
Row MD: The red areas show white matter where
the overall rate of water diffusion was higher than in typical children,
also indicating abnormal white matter.
Row RD: The red areas
show white matter where SPD children have higher rates of water
diffusion perpendicular to the axonal fibers, indicating a loss of
integrity of the fiber bundles comprising the white matter tracts.
The study examined 16 boys, between the ages of eight and 11, with
SPD but without a diagnosis of autism or prematurity, and compared the
results with 24 typically developing boys who were matched for age,
gender, right- or left-handedness and IQ. The patients’ and control
subjects’ behaviors were first characterized using a parent report
measure of sensory behavior called the Sensory Profile.
The imaging detected abnormal white matter tracts in the SPD
subjects, primarily involving areas in the back of the brain, that serve
as connections for the auditory, visual and somatosensory (tactile)
systems involved in sensory processing, including their connections
between the left and right halves of the brain.
“These are tracts that are emblematic of someone with problems with
sensory processing,” said Mukherjee. “More frontal anterior white matter
tracts are typically involved in children with only ADHD or autistic
spectrum disorders. The abnormalities we found are focused in a
different region of the brain, indicating SPD may be neuroanatomically
distinct.”
The researchers found a strong correlation between the
micro-structural abnormalities in the white matter of the posterior
cerebral tracts focused on sensory processing and the auditory,
multisensory and inattention scores reported by parents in the Sensory
Profile. The strongest correlation was for auditory processing, with
other correlations observed for multi-sensory integration, vision,
tactile and inattention.
The abnormal microstructure of sensory white matter tracts shown by
DTI in kids with SPD likely alters the timing of sensory transmission so
that processing of sensory stimuli and integrating information across
multiple senses becomes difficult or impossible.
“We are just at the beginning, because people didn’t believe this
existed,” said Marco. “This is absolutely the first structural imaging
comparison of kids with research diagnosed sensory processing disorder
and typically developing kids. It shows it is a brain-based disorder and
gives us a way to evaluate them in clinic.”
Support SPD Research
Thanks to groundbreaking work from UCSF Benioff Children’s Hospital
San Francisco, a biological basis for SPD has been discovered. There is
much work to be done and a funding gap. We still need to:
- Understand the genetic causes of sensory processing differences
- Uncover risk factors for SPD
- Measure the neurologic brain differences in affected individuals
- Determine if current interventions are truly effective for brain plasticity
- Develop new therapies based on scientific evidence
You can pave the way for a new era of sensory research and therapies by supporting UCSF’s scientific sensory processing team.
Learn how you can help.
Future studies need to be done, she said, to research the many
children affected by sensory processing differences who have a known
genetic disorder or brain injury related to prematurity.
The study’s co-authors are Shivani Desai, BS, Emily Fourie, BS, Julia
Harris, BS, and Susanna Hill, BS, all of UCSF, and Anne Arnett, MA, of
the University of Denver.
The research was supported by the Wallace Research Foundation. The
authors have reported that they have no conflicts of interest relevant
to the contents of this paper to disclose.
UCSF Benioff Children’s Hospital creates an environment where
children and their families find compassionate care at the forefront of
scientific discovery, with more than 150 experts in 50 medical
specialties serving patients throughout Northern California and beyond.
The hospital admits about 5,000 children each year, including 2,000
babies born in the hospital. For more information, visit
www.ucsfbenioffchildrens.org.
UCSF is a leading university dedicated to promoting health worldwide
through advanced biomedical research, graduate-level education in the
life sciences and health professions, and excellence in patient care.